Bariatric Surgery
What is Bariatric Surgery?
Bariatric surgery refers to a group of surgical procedures performed to help individuals with severe obesity achieve significant weight loss. The goal of bariatric surgery is to improve the patient’s overall health by reducing excess weight, improving obesity-related conditions (such as type 2 diabetes, hypertension, and sleep apnea), and enhancing quality of life. Bariatric surgery works by modifying the digestive system to either limit food intake, reduce nutrient absorption, or both.
There are several types of bariatric surgery, and the choice of procedure depends on the patient’s health, preferences, and the recommendation of the healthcare team. The most commonly performed types of bariatric surgery include:
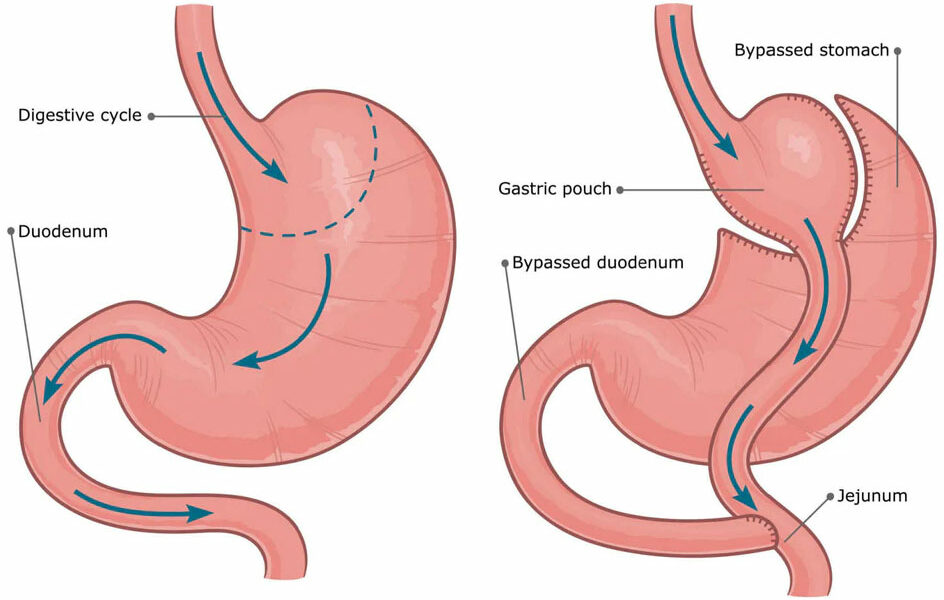
- Gastric Bypass (Roux-en-Y Gastric Bypass): A procedure where the stomach is divided into a small upper pouch and a larger lower pouch, and the small intestine is rerouted to the small pouch.
- Sleeve Gastrectomy (Gastric Sleeve): Involves the removal of a portion of the stomach, leaving a tube-like structure or “sleeve” that limits food intake.
- Adjustable Gastric Banding (Lap-Band): A band is placed around the upper part of the stomach to create a small pouch that limits food intake.
- Biliopancreatic Diversion with Duodenal Switch (BPD/DS): A more complex surgery that involves removing part of the stomach and bypassing a large portion of the small intestine to limit both food intake and nutrient absorption.
- Endoscopic Procedures: These include non-surgical methods such as intragastric balloons, where a balloon is placed in the stomach to limit space for food and promote weight loss.
Bariatric surgery has been shown to significantly reduce the risk of obesity-related conditions, such as heart disease, diabetes, and certain cancers. However, it is not a quick fix, and successful weight loss requires lifelong commitment to dietary changes, exercise, and regular follow-up care.
Causes for Bariatric Surgery
Bariatric surgery is typically recommended for individuals who have not been successful in achieving sustained weight loss through other means, such as diet and exercise, and who are dealing with obesity-related health problems. Specific causes or criteria for bariatric surgery include:
Severe Obesity (Morbid Obesity):
- Bariatric surgery is typically recommended for individuals with a body mass index (BMI) of 40 or higher, which is considered morbid obesity.
- It may also be recommended for individuals with a BMI of 35 or higher if they have obesity-related health conditions (comorbidities), such as diabetes, hypertension, or sleep apnea.
Obesity-Related Health Conditions:
- Individuals who suffer from obesity-related diseases may be candidates for bariatric surgery. These conditions include:
- Type 2 diabetes: Excess weight contributes to insulin resistance, and weight loss can help improve blood sugar control.
- Hypertension (High blood pressure): Obesity is a major risk factor for high blood pressure, and bariatric surgery can help lower blood pressure.
- Obstructive sleep apnea: Obesity is a leading cause of sleep apnea, and weight loss through surgery can alleviate symptoms.
- Heart disease: Obesity increases the risk of cardiovascular problems, and weight loss can reduce this risk.
- Joint problems: Obesity can lead to joint pain and conditions like osteoarthritis, and weight loss can ease the strain on joints.
- Individuals who suffer from obesity-related diseases may be candidates for bariatric surgery. These conditions include:
Failure of Non-Surgical Weight Loss Methods:
- Bariatric surgery is typically considered after other weight loss methods (such as dieting, exercise, and weight loss medications) have not led to sustained weight loss. Individuals who are unable to maintain weight loss through non-surgical means may benefit from surgical intervention.
Psychological Readiness:
- Successful bariatric surgery requires a commitment to long-term lifestyle changes. Psychological readiness is important, and candidates must demonstrate an understanding of the lifestyle changes necessary after surgery, including dietary modifications, exercise, and regular medical follow-up.
Treatment Options for Bariatric Surgery
Bariatric surgery is not just a weight loss procedure; it is a treatment for obesity and related health conditions. The treatment options vary depending on the type of bariatric surgery performed. Below are the most common types of bariatric surgery:
Gastric Bypass (Roux-en-Y Gastric Bypass):
- Procedure: The stomach is divided into a small upper pouch and a larger lower pouch. The small intestine is then rerouted to the small pouch, bypassing the larger portion of the stomach.
- Effectiveness: This surgery is effective for substantial weight loss and has been shown to improve or resolve many obesity-related conditions, such as diabetes and hypertension.
- Benefits: Rapid weight loss, improvement in comorbidities, and the potential for long-term success.
- Risks: It is a more complex procedure and may lead to complications like nutrient deficiencies, dumping syndrome (a condition where food moves too quickly into the small intestine), or bowel obstruction.
Sleeve Gastrectomy (Gastric Sleeve):
- Procedure: A large portion of the stomach is removed, leaving a tube-like structure that limits food intake. The small intestine remains intact, so nutrient absorption is not significantly altered.
- Effectiveness: It leads to significant weight loss and improvement in obesity-related diseases. It is one of the most popular bariatric surgeries due to its simplicity and effectiveness.
- Benefits: No rerouting of the intestines, less complicated than gastric bypass, and effective for weight loss.
- Risks: Potential for acid reflux, and nutrient deficiencies may develop over time.
Adjustable Gastric Banding (Lap-Band):
- Procedure: A silicone band is placed around the upper portion of the stomach to create a small pouch, limiting food intake. The band can be adjusted to control the size of the stomach opening.
- Effectiveness: This method has a slower rate of weight loss compared to other procedures but can still be effective if combined with lifestyle changes.
- Benefits: It is reversible and adjustable, which allows for flexibility in managing weight loss.
- Risks: It may lead to complications like band slippage, esophageal dilation, or pouch enlargement, and the weight loss may not be as significant as with other procedures.
Biliopancreatic Diversion with Duodenal Switch (BPD/DS):
- Procedure: This is a more complex surgery that involves the removal of a large portion of the stomach (similar to the sleeve gastrectomy) and rerouting the intestines to bypass a significant portion of the small intestine, which reduces nutrient absorption.
- Effectiveness: This procedure leads to significant weight loss and is highly effective in treating obesity-related diseases.
- Benefits: It leads to substantial and rapid weight loss and can improve or resolve comorbidities.
- Risks: There are significant risks of nutrient deficiencies, requiring lifelong vitamin supplementation, and it is a more complex procedure than others.
Endoscopic Bariatric Procedures:
- Intragastric Balloon: A balloon is inserted into the stomach using an endoscope and inflated to reduce the amount of space available for food. This helps individuals eat less and feel full sooner.
- Effectiveness: This is a less invasive option than surgery and can help with weight loss, but it generally leads to a smaller amount of weight loss compared to surgical methods.
- Benefits: It is minimally invasive, can be performed in an outpatient setting, and does not involve cuts or incisions.
- Risks: Potential for nausea, vomiting, or discomfort. The balloon must be removed after six months.
Tests and Evaluation for Bariatric Surgery
Before undergoing bariatric surgery, patients are carefully evaluated to determine whether they are suitable candidates for the procedure. The evaluation process typically involves:
Medical History and Physical Exam:
- A thorough review of the patient’s medical history, including obesity-related health conditions, previous weight loss attempts, and current medications, is essential.
- A physical exam helps assess the patient’s overall health and identify any potential issues that could complicate surgery.
Psychological Evaluation:
- Since bariatric surgery requires significant lifestyle changes, a psychological evaluation is important to assess the patient’s mental health, readiness for the surgery, and ability to handle the emotional and psychological challenges of the process.
- It may include assessing for eating disorders, depression, or other mental health conditions.
Nutritional Assessment:
- A dietitian will evaluate the patient’s current diet, eating habits, and nutritional status to help tailor dietary recommendations both before and after surgery.
- Ensuring adequate nutrition is especially important after bariatric surgery, as nutritional deficiencies can arise.
Laboratory Tests:
- Blood tests are conducted to assess the patient’s overall health, check for conditions like anemia or diabetes, and evaluate liver and kidney function.
- Tests may include glucose levels, cholesterol levels, and vitamin/mineral deficiencies.
Imaging and Diagnostic Tests:
- Imaging tests such as an abdominal ultrasound, X-ray, or endoscopy may be used to evaluate the stomach and other organs for any structural issues.
- An endoscopy or upper GI series may be used to check for conditions like hernias or ulcers that could affect surgery.
Sleep Study:
- If the patient has symptoms of sleep apnea (such as loud snoring or daytime fatigue), a sleep study may be recommended to diagnose this condition, which can be worsened by obesity and complicate surgery.
Conclusion
Bariatric surgery is a highly effective treatment option for individuals struggling with severe obesity and related health conditions. It can significantly improve quality of life, reduce the risk of obesity-related diseases, and lead to substantial weight loss. However, it requires careful consideration, including medical and psychological evaluation, as well as long-term commitment to lifestyle changes such as diet and exercise. Patients should work closely with a multidisciplinary healthcare team to determine the best treatment option and ensure successful outcomes from the surgery.